"Navigating the Lifelines: Strategies for Managing Kidney Chaos"
- Dr Vivek Viswanathan

- Mar 27, 2024
- 8 min read
Updated: Apr 9, 2024
The marvels of modern medicine that keep the rhythm of life pulsing in tiny bodies.
Renal Replacement Therapy
Chronic Kidney Disease

Chronic Kidney Disease (CKD) in children is a serious condition that requires comprehensive understanding and management. It is a long-term, progressive disease that gradually damages the kidney's ability to function properly. The kidneys play an essential role in the body, filtering waste products from the blood and excreting them in urine. They also help regulate blood pressure, red blood cell production, and the balance of calcium and other minerals in the body. When the kidneys are not functioning efficiently, harmful levels of fluid and waste can build up in the body, leading to a host of health complications.

The causes of CKD in children vary, but common ones include congenital malformations, genetic disorders, systemic diseases, and obstruction or reflux. Some children are born with kidney malformations that lead to CKD, while others may develop the condition due to diseases that affect the kidney, such as diabetes or lupus. Urinary tract problems, such as blockages or reflux, can also lead to CKD if they cause long-term damage to the kidneys.

Diagnosing CKD in children can be challenging as the symptoms often appear late in the disease or are non-specific. These may include poor growth, lack of appetite, fatigue, frequent urination, high blood pressure, or swelling in the hands and feet. The diagnosis is usually confirmed through blood and urine tests that measure the levels of waste products, electrolytes, and protein. Imaging tests, such as ultrasound or CT scan, can also provide valuable information about the size and structure of the kidneys.

Management of CKD in children aims to slow the progression of the disease, relieve symptoms, and prevent complications. This often involves dietary modifications, medications, and in severe cases, dialysis or kidney transplantation. A low-sodium, low-protein diet can help reduce the workload on the kidneys, while medications can help control high blood pressure, correct electrolyte imbalances, and manage anemia. Dialysis is a procedure that artificially filters waste products from the blood when the kidneys can no longer do so.


Kidney transplantation is often the treatment of choice for children with end-stage renal disease (ESRD), the final stage of CKD. It involves replacing the diseased kidney with a healthy one from a donor. Kidney transplantation can significantly improve the quality of life and survival rate of children with ESRD, but it also comes with risks and requires life-long medications to prevent the body from rejecting the new kidney.
Living with CKD can be challenging for children and their families. It often requires regular medical appointments, medications, dietary restrictions, and in some cases, home dialysis. It can also affect a child's growth, development, and quality of life, and may cause emotional stress. Therefore, comprehensive care for children with CKD should also involve psychological and social support, and close collaboration among healthcare professionals, the child, and their family.
Dialysis

Dialysis plays a significant role in managing children with severe kidney diseases. It's a life-saving procedure that replicates the function of healthy kidneys when they fail to work properly. Dialysis is a bridge to kidney transplantation or, in some cases, a long-term solution for children who are not suitable for a transplant.
There are two types of dialysis: hemodialysis and peritoneal dialysis. Both methods help to remove waste products and excess fluid from the body, which accumulate when the kidneys are not functioning at full capacity.
Hemodialysis, the more commonly known form of dialysis, involves the circulation of the child's blood through a machine that filters out toxins and excess fluid. The clean blood is then returned to the child's body. This process requires access to the bloodstream, usually through a vascular access known as a fistula or graft, created surgically. Hemodialysis is typically performed in a dialysis center or hospital, and each session lasts around four hours, usually three times a week.

Peritoneal dialysis, on the other hand, uses the child's peritoneum, a natural filter, which is the lining of the abdomen. During this process, a dialysis solution is infused into the peritoneal cavity through a catheter inserted surgically into the abdomen. The solution absorbs waste and excess fluid from the blood, across the peritoneum. After a few hours, the used solution is drained out and replaced with fresh solution, a process known as an exchange. Peritoneal dialysis can be performed at home, school, or while traveling, thus offering greater flexibility for the child and family. Peritoneal Dialysis can be of two types : Continuous ambulatory peritoneal dialysis or automated peritoneal dialysis.

The choice between hemodialysis and peritoneal dialysis depends on various factors such as the child's age, medical condition, lifestyle, and the family's preference.

Younger children and infants are often treated with peritoneal dialysis as it is more suitable for their smaller size and can be managed at home. However, hemodialysis may be used in emergencies to quickly correct electrolyte imbalances or remove toxins.
Regardless of the type of dialysis, children will require careful monitoring to ensure the treatment is working effectively. Regular blood tests are performed to check the levels of waste products and to adjust the dialysis prescription as needed. Managing diet and fluid intake is also crucial in children undergoing dialysis.
Dialysis is not without its challenges. It can be physically exhausting and emotionally draining for the child and family. The procedure can also lead to potential complications such as infections, blood clots, anemia or changes in blood pressure. Therefore, a multidisciplinary team approach is essential to provide comprehensive care for the child, addressing not only the medical needs but also the psychosocial aspects.
In conclusion, dialysis is a critical component of paediatric urology, providing a lifeline for children with serious kidney diseases. While it is a complex and challenging procedure, advancements in technology and care practices continue to improve the quality of life for these children, enabling them to lead active and fulfilling lives.
Renal Transplantation
Renal transplantation holds a significant role, offering a new lease of life to children suffering from end-stage renal disease. This complex surgical procedure involves the replacement of a dysfunctional kidney with a healthy one, often sourced from a live or deceased donor. The fundamental objective is to restore kidney function, enabling the child to lead a normal, healthy life.
The decision to proceed with renal transplantation is usually taken when a child's kidney function falls below 15-20%, a stage classified as end-stage renal disease (ESRD). The severity of the situation necessitates immediate medical intervention, with renal transplantation often emerging as the most viable treatment option.
The pre-transplantation process is comprehensive and involves several steps. The patient is first thoroughly assessed to determine their suitability for the surgery. This involves evaluating their overall health status, including cardiovascular fitness, nutritional status, and psychological well-being. The compatibility between the donor and recipient is also assessed, taking into account factors such as blood type and tissue type.

The surgery itself is a complex procedure. The new kidney is placed in the lower abdomen, with the blood vessels of the kidney connected to the recipient's blood vessels. The ureter of the donor kidney is then connected to the bladder to allow for the passage of urine. The diseased kidneys are usually left in place unless they are causing complications.
Post-transplant, the child is closely monitored for any signs of rejection. Immunosuppressive drugs are administered to prevent the body from rejecting the new kidney. These medications, while crucial, can have side effects including increased susceptibility to infections and certain types of cancer, necessitating regular follow-ups and adjustments of medication dosage.
Renal transplantation in children differs from adults due to the unique challenges presented by the paediatric population. Children have smaller body sizes, making the surgical procedure more intricate. Additionally, they may have congenital anomalies or developmental issues that further complicate the process.
Another major consideration in paediatric renal transplantation is growth. Kidney disease and long-term dialysis can hinder a child's growth. A successful renal transplant can improve growth by restoring kidney function. However, the use of immunosuppressive drugs can potentially affect growth and development, necessitating careful monitoring and adjustment of medication.
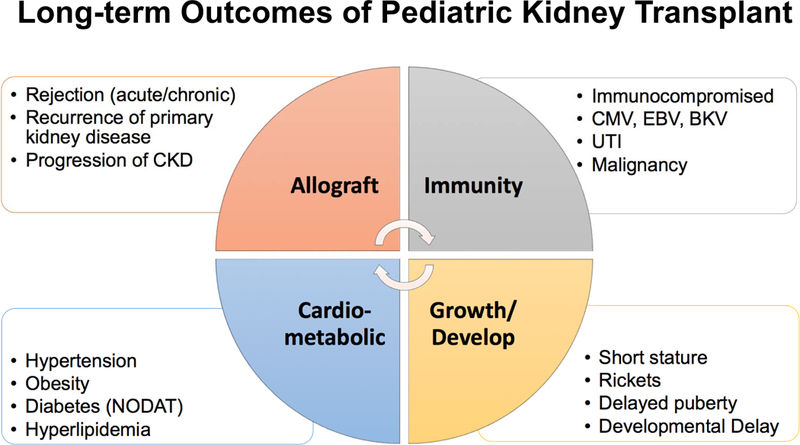
Psychosocial aspects also play a significant role in paediatric renal transplantation. The child and their family must cope with the diagnosis and the prospect of significant surgery. Post-transplant, adherence to medication regimes and regular medical follow-ups become a vital part of their lives. Support from healthcare professionals, social workers, and psychologists can help the child and their family navigate these challenges.
In conclusion, renal transplantation is a life-saving procedure for children with end-stage renal disease. It involves a complex interplay of surgical, medical, and psychosocial elements, each of which must be carefully managed to ensure the best possible outcome for the child. Despite the challenges, with appropriate care and support, many children who undergo renal transplantation can look forward to a healthier and more fulfilling life.
Living with Renal Disease
Renal diseases present unique challenges and significant impacts on a child's life. A renal disease, often considered a silent killer, is a severe condition that affects the kidneys' functionality. The kidneys, two bean-shaped organs located at the back of the abdomen, play a pivotal role in maintaining the body's overall health by filtering wastes and excess fluids from the blood. When a child is diagnosed with a renal disease, it means that these vital organs are not functioning as they should, leading to various health complications.
Living with a renal disease is a life-altering experience, particularly for children. They face a multitude of challenges, including physical discomfort, dietary restrictions, frequent medical visits, and the emotional stress of coping with a chronic illness. Children with renal disease may experience symptoms such as fatigue, difficulty in concentrating, loss of appetite, and growth retardation, all of which can significantly impact their quality of life.
One of the most critical aspects of managing renal disease is dietary modification. Children with renal diseases often need to follow a strict diet to prevent further damage to their kidneys. Their diet typically involves limiting the consumption of proteins, sodium, and potassium, which can be challenging for children who crave a variety of foods. Parents and caregivers must ensure that such dietary restrictions are adhered to without compromising the child's nutritional needs.


In addition to dietary changes, children with renal diseases often require various medications to manage their symptoms and slow the progression of the disease. These medications can range from supplements to replace deficiencies caused by the disease, to drugs that help control blood pressure and cholesterol levels. Taking medication regularly and at precise times can be particularly challenging for children, requiring a significant amount of discipline and understanding.
Regular medical visits are also a part of life for children with renal diseases. These visits often involve blood tests, urine tests,

imaging studies to monitor the disease's progression and assess the effectiveness of treatments. While these visits are crucial for managing the disease, they can cause anxiety and stress in children.
Living with a renal disease can also have profound psychological impacts on children. The constant worry about their health, the restrictions on their lifestyle, and the frequent medical visits can lead to feelings of anxiety, depression, and social isolation. Therefore, psychological support is an essential part of the treatment plan for children with renal diseases. This support can come from various sources, including psychologists, social workers, and support groups for children with similar conditions.

Despite these challenges, it's important to remember that a diagnosis of renal disease is not the end of the world. With proper management and care, many children with renal diseases can lead fulfilling lives. Advances in paediatric urology have led to improved treatment options and better quality of life for children with these conditions. Living with a renal disease may be a lifelong journey, but with support, understanding, and appropriate care, children can navigate this journey successfully.
















Comments